
Floribunda
2024

Harebells (Campanula rotundifolia)
2021

Hand-painted ukulele
2021


Ring of Fire
Watercolor, colored pencil, 16 x 12. Helianthus annus
2020

Daffodils & Ferns
Watercolor, 16 x 12. An ode to the bittersweet, anxious, but beautiful springtime of 2020.
2020

Hydrangea Leaf Buds 10X
Colored pencil with watercolor on paper. 9 x 12. SOLD
2020

Tulip tree - Liriodendron tulipifera
Watercolor 11 x 14 SOLD
2020

English Elm
Watercolor
2020

Florida fighting conch (Strombus alatus)
Watercolor, graphite, colored pencil.
2019

November's Holly
Graphite and watercolor
2019

Ornamental Gourd
Watercolor, with colored pencil
2019
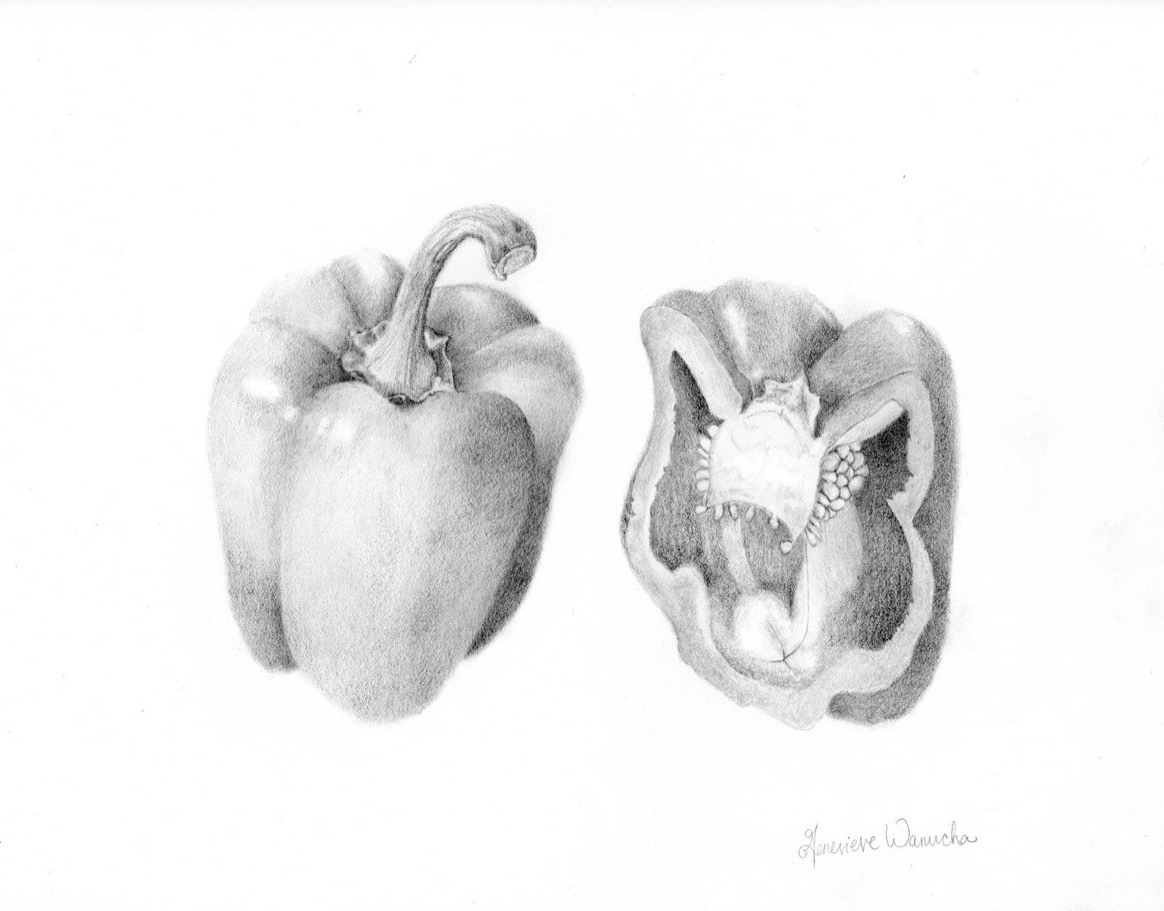
Red Bell Pepper, Inside and Out
Graphite
2019
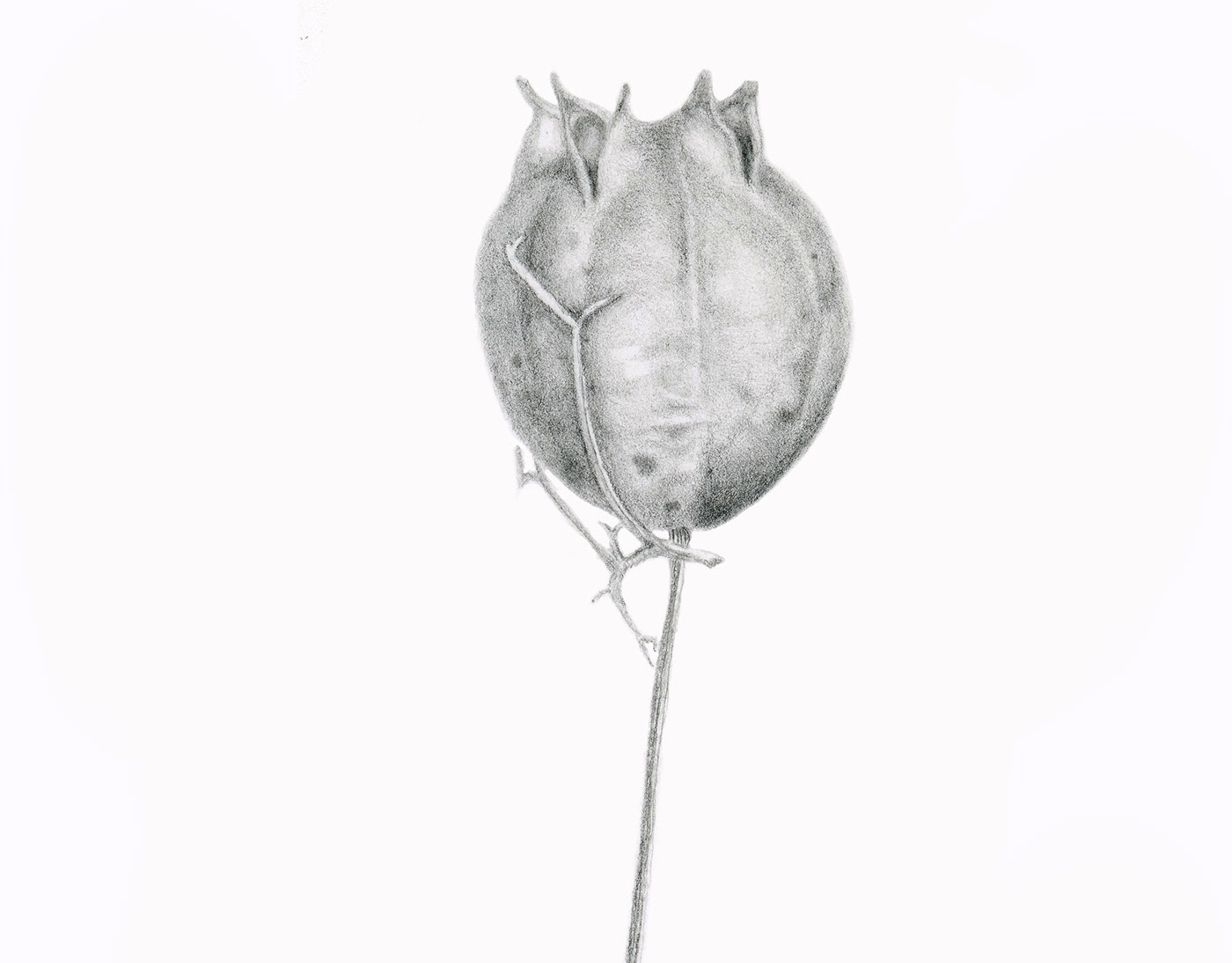
Nigella seed pod, dried, 200%
Graphite
2019

Atlantic Knobbed Whelk, Duxbury, MA
Colored pencil, graphite
2019

Black bear
Color pencil
2019
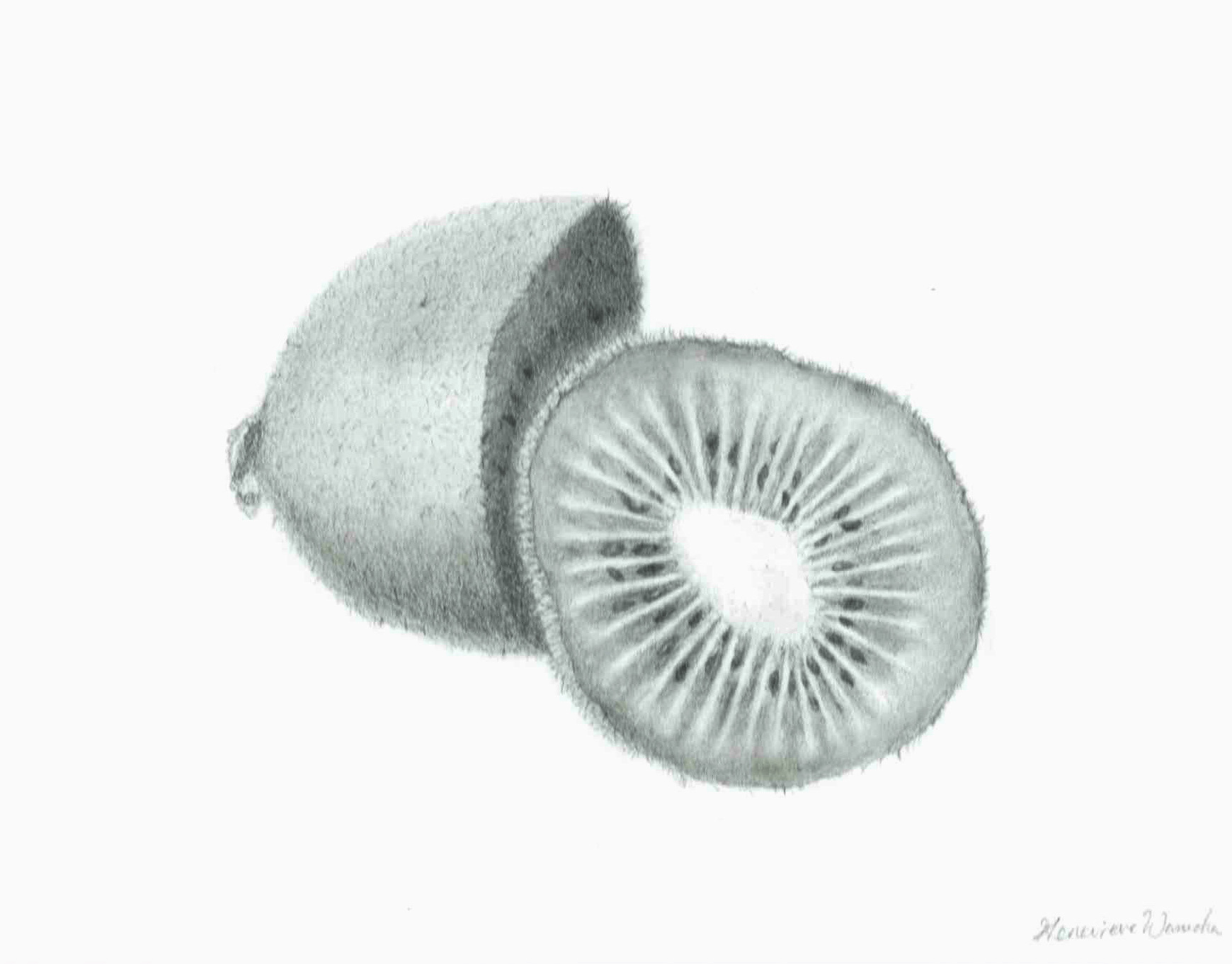
Kiwi
Graphite
2018
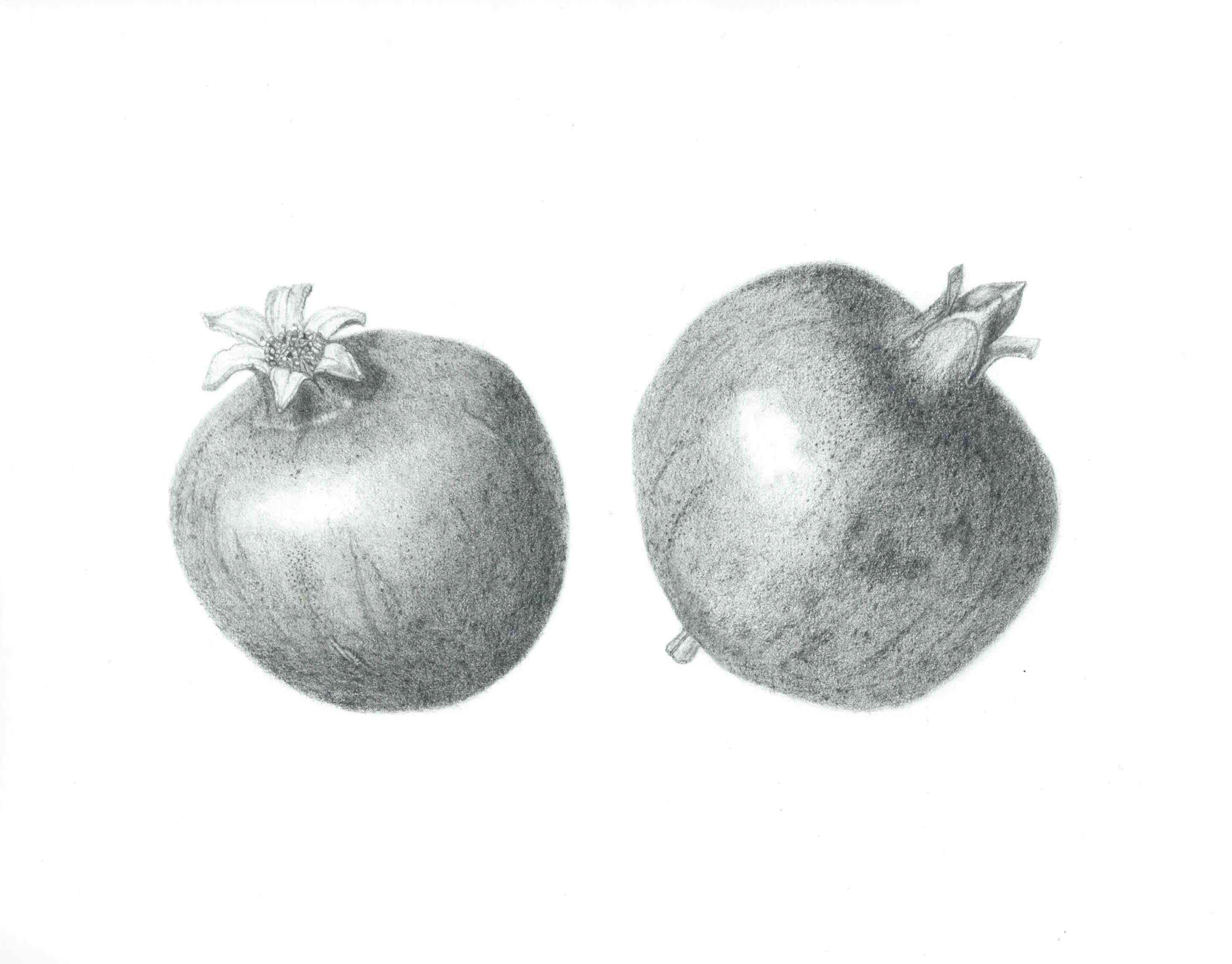
Pomegranates of a Healdsburg, CA Home Garden
Graphite
2018

Allium cepa
Watercolor
2019
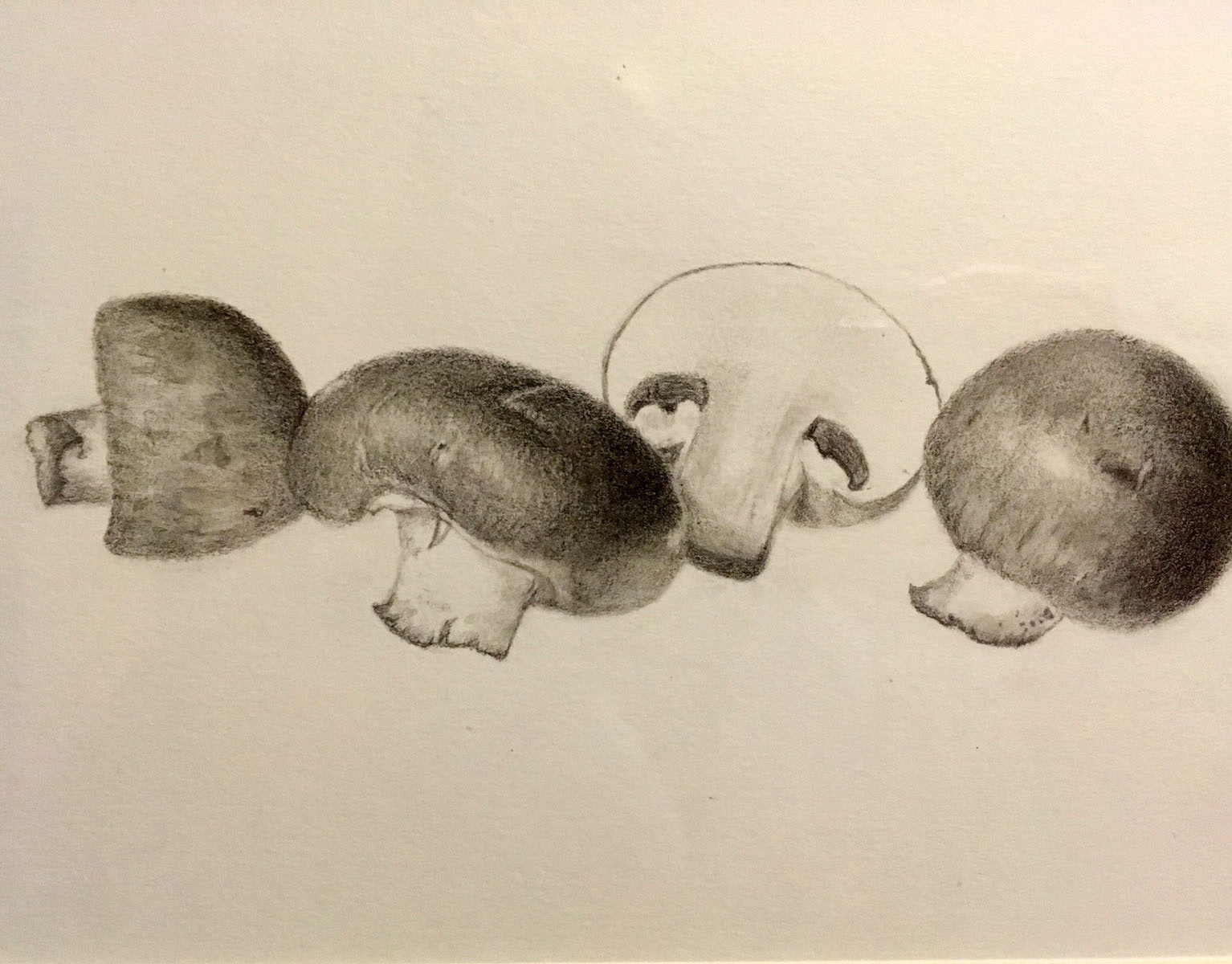
Criminis
Graphite
2019